INTERVENTIONAL ONCOLOGY; CANCER DIAGNOSIS AND TREATMENT

Interventional radiology
Interventional radiology plays a crucial role in the clinical management of cancer patients, offering less invasive alternatives to traditional surgical methods. Let’s delve into the details:
- Diagnosis Stage:
- When imaging methods detect a disease (such as a tumor) within an organ, interventional radiologists step in. They obtain tissue samples using techniques like ultrasonography or computed tomography (CT).
- These samples help confirm the diagnosis and guide subsequent treatment decisions.
- Treatment Phase:
- Interventional radiology collaborates closely with oncology departments during the treatment phase.
- For patients with limited response to chemotherapy, interventional procedures become essential.
- Interventional Oncology Treatment Methods:
- Tumor Ablation:- Various needle-based techniques directly target the tumor:
- Radiofrequency (RF) Ablation: Heat is applied to burn the tumor
- Microwave Ablation: Microwaves are used to destroy the tumor.
- Cryoablation: The tumor is frozen.
- Chemoembolization:- Chemotherapeutic drugs are delivered directly into the tumor via the artery feeding it (commonly used for liver tumors).
- Radioembolization:- Radioactive material is injected directly into the tumor through the artery.
Imaging-Guided Biopsy
- Purpose: To definitively diagnose diseases.
- Aspiration Biopsy:- Small tissue samples are taken from the diseased organ using a needle.
- Tru-Cut or Partial Biopsy:- Larger tissue samples are obtained for further analysis.
- Process Preparation: Before performing a tissue biopsy, certain blood tests are necessary. Once the most suitable entry point for the lesion is determined, the skin is prepared under sterile conditions, and local anesthesia is applied to the skin and subcutaneous tissue.
In cases where a biopsy is needed for masses that cannot be visualized using ultrasonography, computerized tomography (CT) is utilized.
It’s important to note that bleeding, infection, and injury to adjacent organs are potential risks associated with the procedure. However, these risks can be significantly reduced by conducting blood tests prior to the procedure, assessing the patient’s medication history, maintaining sterile conditions, and carefully approaching the access site.
Port Placement
Chemotherapy drugs can cause damage to the veins in the arms over time. As a result, these veins become unsuitable for administering further chemotherapy treatments.
To address this issue, a port placement procedure is performed in the angiography unit under ultrasonography guidance within interventional radiology departments.
The port placement is carried out under sterile conditions and local anesthesia. After creating a catheter entry through the neck veins, the port pocket is formed. The port is then implanted under the skin and sutured in place. Importantly, since the port is situated beneath the skin, there is no external component.
This design ensures that the patient’s quality of life remains unaffected. The port is easily palpable under the skin. Chemotherapy drugs are administered through the port using specific needles.
It’s crucial to use only the designated needle for the port. After each use, the port should be flushed with blood thinners to prevent clogging. Approximately one week later, the stitches from the port placement procedure are removed. Patients with a port can safely take a bath once the stitches have healed.
Local Treatments for Liver Cancers
"Ablation’’ treatment in cancer various treatment methods are applied in tumors. These methods can be listed as “surgery, chemotherapy and radiotherapy” applications.
The classical treatments for lung, liver and kidney tumors are surgery, but most patients miss the chance of surgery because they are not caught at an early stage.
Ablation Treatment in Liver Tumors
Ablation treatment is a treatment that is curative (definitive treatment) in tumors smaller than 3 cm, prevent recurrence of tumor formation in medium-sized HCC between 3-5 cm, extend lifespan, and reduce tumor margins.
Radiofrequency (RF) ablation technique ensures tumor-cell death by converting radiofrequency current into heat energy around an electrode placed inside the tumor. With this treatment, the 5-year survival rate in liver cancer (HCC) cases is 40-58%. Its effectiveness in small and mediumsized HCCs can be up to 80% in a single application. Presence of vessels in the area close to the lesion reduces the ablation efficiency and may prolong the procedure time. Grounding pads need to be used and, rarely, RFA can sometimes cause skin burns.
Microwave Ablation (MW) is a thermal treatment method that is widely used particularly in liver tumors. The MWA system can directly and laparoscopically be used on the skin (percutaneous) as well as in open surgery. The MWA technique has some advantages compared to the RF ablation: it can create a larger ablation area, does not require grounding pads, and is more effective in ablation of tumors located close to vessels.
Other ablation techniques in liver cancer, cryoablation (CRYO), irreversible electroporation, high-intensity focused ultrasound ablation (HIFU), laser ablation and ethanol ablation treatments are also performed.
How is Ablation Applied?
After the evaluation of blood tests, the location of the lesions are shown using ultrasonography, computed tomography and magnetic resonance imaging methods, and the location and number of interventions are determined. Ablation is most commonly performed directly through the skin and is usually accompanied by ultrasonography or a computerized tomography device.
In addition to neuroendocrine tumors, ablation treatments are also effective in the spread of breast and ovarian cancers to the liver, in cases where surgery is not applied.
Tumors of other organs other than the liver; Ablation techniques are also important treatment methods in lung, kidney cancer and bone metastases.
It can be a treatment alternative to relieve pain in cases of painful bone tumor spread (metastasis).
Chemoembolization
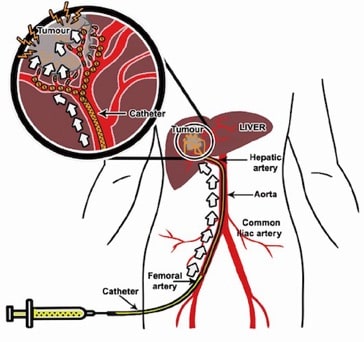
Chemoembolization is the method of administering chemotherapy drugs directly into the tumor through a catheter by entering the groin artery and reaching the artery in the liver.
Side effects that occur in chemotherapy drugs given systemically are not seen in chemoembolization, since the drug does not mix with the systemic circulation, systemic side effects are not seen or only effects limited to the liver can be seen. In this way, all tumors located in the liver are to be able to be treated.
Chemoembolization can also be applied in patients with liver cancer or metastases coming from other organs to the liver, in patients who failing to respond to systemic chemotherapy and with impaired health status.
The following is required for this treatment:
- Tumor volume should be less than 50% of the entire volume of the liver.
- According to blood tests, albumin, total bilirubin, AST, ALT, LDH values are normal or slightly above normal.
- Evaluation of involvement of other organs other than the liver and the absence of advanced or widespread cancer involvement in these organs.
- The veins that feed the liver must be open. Depending on the extent of the tumors located in the liver, treatment can be done in a single or several sessions.
Radioembolization
Radioembolization is an effective treatment method that has been used in recent years. It is based on application of radioactive substance (Yttrium 90) into the groin artery and directly to the tumor via the liver artery.
In external radiotherapy, that is, outside the skin, normal liver tissue is seriously damaged at a dose that will kill the tumor. For this reason, radioembolization, a safer method, has become the main treatment method that can be applied in cases that develop resistance to chemotherapy.
In which cases can radioembolization primarily be applied?;
- HCC (hepatocellular carcinoma), cancer that develops primarily in the liver.
- Metastases to the liver from large intestine, breast cancer, and neuroendocrine tumors.
- It can also be an alternative treatment method for bile duct cancer (cholangiocarcinoma) for which surgery is not possible.
- Radioembolization can also be performed if chemoembolization cannot be applied in case of obstruction of the liver veins.
How is radioembolization treatment performed? In this practice, carried out together with the Nuclear Medicine unit, the treatment is performed at the angiography unit in 2 separate sessions. The 1st session is performed to determine the vascular structure of the tumor and calculate the dose. The 2nd session angiography is performed approximately 1 or 2 weeks later. The dosed Yttrium 90 is directly applied to the target tumor. Depending on the extent of the tumor,
After the treatment, symptoms such as nausea, vomiting and fever may last for about 1 day. Radiation-induced liver disease may occur in 50% of cases and may cause elevated blood tests and last up to 2 weeks. Radiation pneumonitis is a rare condition that may occur in cases where leakage to the lungs is higher. Ulcer development in the stomach and intestines, inflammation of the pancreas, and inflammation of the gallbladder are rare side effects.
Supportive Interventional Methods in Oncology
Bile Duct Obstruction Drainage
When cancer-related jaundice occurs due to bile duct obstruction, it’s crucial to address this issue promptly. In cases where the endoscopic retrograde cholangiopancreatography (ERCP) technique is not feasible (due to previous gastrointestinal surgery, technical limitations, or other reasons), alternative approaches are used. One such method involves percutaneous drainage.
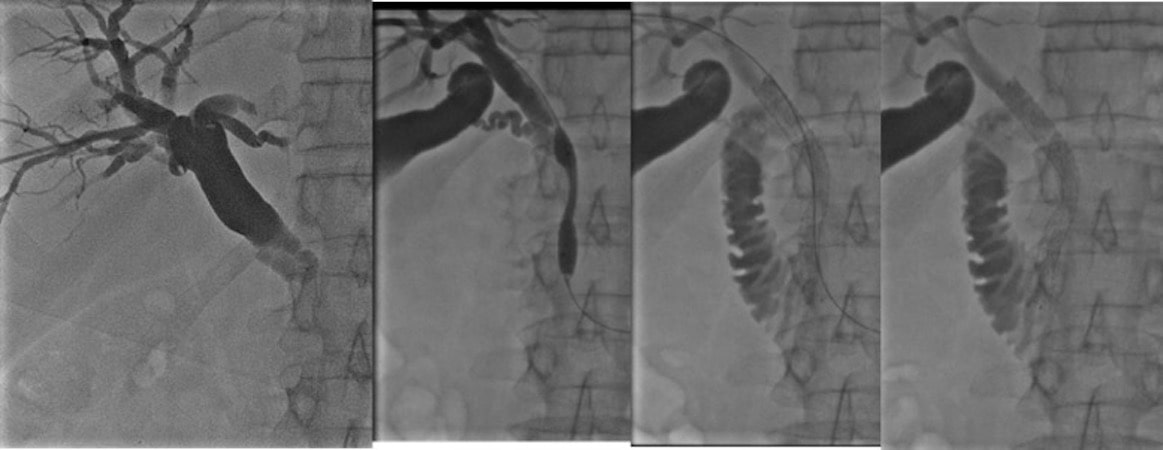
A 60 years old man with biliary obstuction. Baloon and stenting were done to relive of obstruction. After treatment biliary fluid was able to flow into intestine freely.
Here, a catheter is inserted directly through the skin and into the bile ducts to relieve the obstruction. This procedure helps improve patient quality of life and prevents life-threatening complications.
Urinary Tract Obstruction Drainage
When urine flow is obstructed within the urinary tract, it can lead to kidney enlargement and impaired kidney function.
Common causes of urinary tract obstruction include stones, inflammatory conditions, tumors, and ureteral injuries resulting from prior surgeries.
Treatment options depend on the specific cause and may involve interventions to remove or bypass the obstruction.
Cyst and Collection Drainages:
During cancer treatment, patients may develop fluid collections, such as ascites (abdominal fluid), pleural effusion (fluid around the lungs), lymphoceles, or abscesses.
To manage these conditions, interventional radiologists can place a catheter directly into the affected area. Ultrasonography or computed tomography (CT) guidance ensures accurate placement of the catheter.
This drainage procedure helps alleviate symptoms and improve patient comfort.


