PELVIC CONGESTION SYNDROME - PELVIC VENOUS INSUFFICIENCY
Pelvic Pain
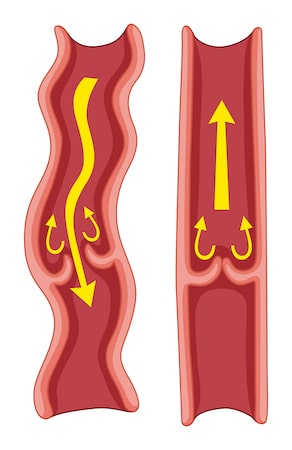
Pelvic Congestion Syndrome (PCS), also known as pelvic venous insufficiency, is a chronic pain condition associated with blood flow problems in the pelvic veins. The pain lasts longer than 6 months and isn’t linked to either the menstrual cycle or pregnancy. Let’s delve into the details:
Symptoms
- The pelvic pain experienced with PCS can vary from dull and achy to sharp and intense.
- Pain may be localized on the left side (most common), right side, or both.
- It often starts during or after pregnancy and may worsen with subsequent pregnancies.
- Other symptoms include varicose veins in the pelvis, buttocks, thighs, vulva, and vagina.
- Frequent bouts of diarrhea and constipation (irritable bowel).
- Accidental urination during laughing, coughing, or other movements (stress incontinence).
- Pain during urination (dysuria).

Causes and Risk Factors
- The exact cause of PCS remains uncertain, but changes in blood flow within the ovarian veins and pelvic veins play a role.
- Risk factors include varicose veins: enlarged veins in the legs.
- Family history of varicose veins.
- Polycystic ovarian syndrome (PCOS).
- Multiple pregnancies (having given birth more than once).
- It’s rare for postmenopausal individuals to develop pelvic congestion syndrome.
Diagnosis
In patients with leg varicose veins, underlying PCS may persist even after treatment. If leg varicose veins recur despite treatment, consider investigating pelvic congestion syndrome. Remember, PCS is a complex condition, and its management involves a multidisciplinary approach. If you suspect PCS, consult a healthcare professional for proper evaluation and personalized care.
Chronic pelvic pain can significantly impact a person’s quality of life. When evaluating this condition, imaging plays a crucial role in identifying potential causes. Let’s delve into the imaging modalities used for assessing chronic pelvic pain:
- Pelvic Ultrasound:
- Transabdominal and endovaginal approaches are commonly employed.
- Ultrasound is the first-line imaging modality for chronic pelvic pain.
- It helps visualize pelvic structures, including the uterus, ovaries, and surrounding tissues.
- Ultrasound is particularly useful for assessing gynecological conditions such as endometriosis, adenomyosis, and fibroids
- Magnetic Resonance Imaging (MRI):
- MRI serves as an adjunct test when ultrasound findings are inconclusive or when deeper evaluation is necessary.
- It provides detailed images of soft tissues, making it valuable for assessing conditions likedeep invasive endometriosis.
- MRI is superior to ultrasound in visualizing complex pelvic anatomy and identifying abnormalities
- Venography:
- Venography is a definitive diagnostic method.
- It involves inserting a catheter into a vein (usually arm, groin, or neck veins) and administering contrast material.
- Venography helps visualize blood vessels, including varicose veins.
- Findings may include enlargement of the renal vein, retrograde leakage of the ovarian vein and pelvic and thigh varicose veins
Remember that accurate diagnosis is essential for effective treatment. Consultation with a healthcare provider and appropriate imaging can guide management strategies for chronic pelvic pain
Treatment
Treatment for ovarian vein leakage-reflux involves several approaches, and I’ll provide some insights based on the information you’ve shared:
- Coil Embolization:
- Coil embolization is a commonly used treatment method. It aims to address unilateral or bilateral ovarian veins that are leaking or experiencing reflux.
- During this procedure, small metal coils are inserted into the affected veins to block blood flow. The decision may involve closing only the leaking ovarian veins or both veins in the same session.
- Coil embolization typically provides relief for patients, improving their symptoms by 70% to 100%.
- Sclerosing Medication:
- Before coil embolization, some patients receive an injection of sclerosing medication into pelvic varices (dilated veins). This additional step helps enhance the effectiveness of the treatment.
- Stent Placement:
- In cases where syndromes cause pressure on theleft renal vein or iliac vein, a stent can be used to relieve the pressure.
- Stents are small mesh-like tubes that help keep the veins open and maintain proper blood flow.
Complications and Negative Effects:
While endovascular methods (such as embolization) are generally safe, there are some risks such as coil migration. Although rare, there’s a possibility that coils placed in ovarian or pelvic veins may escape with blood flow and travel to the pulmonary veins seen in about 3-4% of patients.
Post-Embolization Symptoms: Some patients may experience pain, nausea, and vomiting after embolization.
Technical Challenges: Difficulties in placing the catheter into the target vein or inadvertent perforation of the ovarian vein can occur, affecting treatment success.
Remember that individual responses to treatment can vary, and it’s essential to discuss these options thoroughly with your healthcare provider. If you have any further questions or need clarification, feel free to ask and call our phone numbers.


